Lip and Tongue Tie
Lip Tie: Infant or Child | Tongue Tie: Infant or Child
Lip Tie
Infant
What is a lip tie?
Lip frenulum’s (maxillary frenulum) are located between the upper jaw or maxilla and the inside of the upper lip. These lip frenulum’s can be broken down into 4 categories, but the most important aspect, in regard to breastfeeding, is how the frenulum impacts the ability for the lip to flange and function. The frenulum can vary in thickness, length and connection point from the lip and upper jaw. As you can imagine with so many variables trying to precisely diagnose a lip tie can be complex.
When assessing an infant to determine if a lip frenulum is negatively impacting nursing a simple exam to assess the range and ease of lip motion can be performed. The infant’s upper lip should roll out and up towards the tip of the nose with little resistance and minimal to no blanching of the frenulum in the area of where it connects to the maxilla. If the lip functions well, it will roll back, and the tip of the lip will be able to contact or come into very close contact with the nose tip. During nursing the infant must breathe through their nose and the lip does not even need to flange back as far as the tip of the nose.
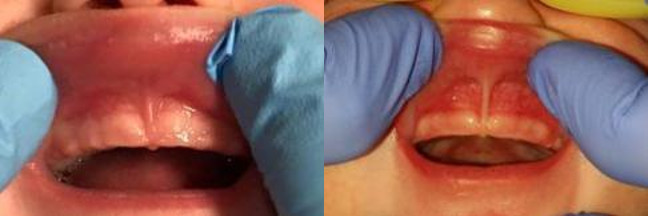
Both of these labial frenulums allow for the upper lip to flange up and back towards the nose with little to no resistance and do not blanch the gum tissue. These are normal and functional frenulums.
If during the exam of the upper lip, the lip is unable to flange to just shy of the tip of the nose and blanching is seen on the gentle rolling back of the lip, the lip frenulum may be restricted and negatively impact the seal or ability for the mouth to have a wide gape or opening.
These labial frenulums are tighter and more restricted as the lip is reflected up and back towards the nose. Notice the blanching or white area in the gums and inability to roll up and back with ease.
What should breastfeeding be like for the infant?
You will learn to understand your infants hunger cues and behaviors in the first weeks of life. The infant will typically eat on a very set schedule and nursing sessions should be efficient and not take excessive amounts of time. Longer nursing sessions can burn valuable calories and cause irritation to the mother’s breasts. The latching of the infant may take a few tries to establish a proper latch, but once established should only require subtle adjustments. The mouth should open wide and accept the nipple and areola with a wide gape or opening. The tongue will grasp, stabilize and draw the nipple into the mouth and create a vacuum, which will elongated the nipple to the back of the infant’s mouth. Once the milk starts to flow, the tongue will continue the wave-like motion to maintain the vacuum and depth of latch. The infant will make a suck or two and then an audible swallow should be heard as the milk is swallowed. The sounds of “gulping” and “clicking” can signify a poor vacuum is in place and the child is swallowing more air then milk. The infant’s hands should be open and relax and eye contact maintained with the mother. Frustration, fatigue and quickly falling asleep at the breast are behaviors that are not common with an efficient and effective nursing infant. After feeds, the baby should be fairly easy to burp and be satiated and happy. Other common problems and concerns regarding the newborn are outlined below and talked about in more depth. The baby must have the ability to have a properly functioning tongue and oral motor coordination to efficiently breastfeed. Once a lactation consultant has properly assessed you and your baby and a suspected functional issue exists, you should consider looking further into a tongue and/or lip tie issue.
Why does my child make a clicking or gulping sound when nursing?
The tongue is needed to make a primary seal and the lips help make a secondary seal when nursing. The inability of the tongue to groove and elevate around the nipple and the upper lip to properly flange out does not allow for the baby to make a good seal at the breast. When the upper lip is curled in and remains curled in, this can allow for milk to leak out of the sides of the mouth or for air to be ingested and swallowed by the baby. You may notice small, darker triangles in the corners of the mouth if the lip is not fully flanged. The parent will need to typically flange and adjust the upper lip manually to properly position the upper lip. Even after a revision, the upper lip still may need to manually displaced until prior compensatory habits are unlearned and the facial muscular works less at the breast.
The tongue also plays a part in the maintenance of a seal because it pulls the nipple into the mouth and enables the baby to latch. The tongue needs to extend, groove and cup around the nipple to pull it into the mouth. If a tongue has limited ability to extend and elevate or cup around a nipple, or the finger when examined, this may also contribute to milk leakage and excessive air intake.
The clicking sound that is heard when the infant nurses can be a result of poor elevation of the tongue or a stronger letdown. As the tongue elevates to draw the nipple into the mouth and form a vacuum, the baby needs to maintain a wide open mouth and allow for the tongue to elevate. If the tongue is unable to maintain the elevation, each suck will make a click sound and this occurs as the tongue drops and breaks the vacuum. The infant will gulp air and swallow this when the system is not closed. This clicking and gulping can lead to ingested air and if not properly managed, lead to gassiness, excessive burping and even symptoms of reflux. This is referred to as Aerophagia Induced Reflux (A.I.R.).
The best way to think about it is the mouth has to make a tube, or closed system to effectively draw milk from the breast or bottle. The roof of the mouth or hard palate forms the top half of the tube and the cupped and grooved tongue forms the bottom half of the tube. These two halves must come together or the tube is not formed and no seal is produced.
Why is my baby having excessive gas, hiccups, fussiness or reflux?
Mild degrees of reflux, hiccups, gas and spit up are all normal for a newborn or infant, but the cause can be for a host of reasons and should be explored. These issues may be due to gastrointestinal issues, normal variations in muscle development and tone of the GI system, food sensitivities associated with the mother’s diet or from excess air intake during bottle and/or breastfeeding. If excess air is ingested, it must exit the body either as gas or burping. If the air is burped up, it can bring up stomach acid and cause discomfort and mimic reflux. The excess air can also distend the stomach and cause fussiness and irritation with the child, too. The child’s stomach may be distended or appear fuller when filled with excessive air after a feeding and mimic colic-like symptoms. We refer to this phenomenon of reflux that is caused by excessive air intake during nursing or bottle feeding as Aerophagia Induced Reflux (A.I.R.).
An excessive amount of or very frequent hiccups can be the result of excess air intake while feeding, too. The air intake will distend the stomach and it pushes on the diaphragm, which is the muscle used to fill and empty the lungs. When the stomach places pressure on the diaphragm, its rhythmic cycle can be broken and lead to hiccups, especially after feeding.
How does the procedure work and how long will it take?
After a thorough review of the mother’s feeding history and infant’s feeding history, birth and medical history the infant will be examined. After a full evaluation and discussing treatment options, a signed consent is obtained from the parent and the procedure can proceed. The infant is taken into a treatment room with the doctor and an assistant. The parents will wait in the exam room and review post-operative guidelines and instructions that they are given at the appointment.
The infant will be swaddled in the treatment room and protective eyewear placed on the infant, provider and assistant in the room. Once all eyewear is in place, the laser is turned on. The assistant will help stabilize the infant and maintain the swaddle during the procedure. The type of laser we use is a CO2 Laser and is able to precisely and quickly release the upper lip. The entire procedure to release the upper lip will last about 10 to 15 seconds.
Some infants will benefit from the release of the upper lip to allow for a wider gape and an improved seal while breastfeeding. When revising the upper lip, we grasp the upper lip and gently roll it up towards the nose to reveal the upper lip frenulum. The release of the frenulum from the upper jaw to allow for an improved range of motion of the upper lip.
Post procedural bleeding is typically very rare but may occur and easily managed with light pressure.
Post Revision Wound Management
After the revision of the lip or tongue, the need for active wound care and stretching is mandatory. The reasoning behind these stretching exercises is to help minimize the wound from excessively contracting and tightening as the area heals.
No technique or frequency of stretches has been agreed upon or found to be more or less effective.
If wound site does not look or feel completely healed, at Day 14, continue stretches for one more week. Please see the post revision picture sequence page to see how the wound may heal over the course of 2 weeks.
You will have to try to find the best time to do the stretches for the infant. Stretching between switching breasts, halfway through a bottle OR while changing a diaper are typically the best three options. The stretches should be spaced out evenly through the day.
Stretching of the lip revision site:
The lip stretch is somewhat easier to access then the tongue, but may be slightly more sensitive when stretching. Please refer to the photo below for guidance in regard to the lip exercises.
Once the tongue has been stretched, take the index finger and gently place the finger up under the lip into the area of letter A or B. In a windshield washer motion, take the index finger and wipe it under the lip as you touch the wound site. It should feel smooth as you run you finger from side to side. Take the finger from letter A to letter B and back. Repeat this 4 times. To review: finger under the lip and from A to B and B to A, repeat 4 times.
Remove the finger from the mouth and place the infants head in both open palms. Take your thumbs the gently roll the lip up towards the nose and hold this position for 5 seconds. After rolling the lip back, you have completed the stretches.
Once you are comfortable with the stretches, it will take roughly 20-30 seconds to complete a full set of stretching.

Child
Do lip frenulum's impact speech?
Lip frenulum’s have very little if any impact at all in regard to speech. The upper lip is involved in the “B” and “P” sound and is made as the lips come together in contact. In a normal resting position, the lips should be able to gently touch one another. The tongue can have a much greater impact on speech and jaw development, which will impact speech and articulation more profoundly than any lip frenulum.
One of the most common questions about lip frenulum revolves around a space or gap between the front teeth and the frenulum. Spacing in infant and children’s teeth is extremely beneficial and ideal. These baby teeth that are spread out and have spaces are easier to clean and the space between the baby teeth will be later occupied by the much wider adult teeth. Genetics play a large part in spacing between the front two teeth and is referred to as a diastema. If the child’s parent or grandparent has a prominent space between the two front teeth or the gap was corrected through braces or cosmetic dentistry, the infant will likely have a diastema as well later on in life. Revising or fixing the frenulum as an infant will NOT resolve the genetic cause of this diastema.
How does the lip frenulum effect the teeth and hygiene?
Lip frenulums can present as thicker, shorter and extend over the maxilla and onto the hard palate. At times this specific presentation can lead to great challenges for the parent to brush the upper teeth and can possibly impact the esthetics or smile of the child. It is extremely difficult to predict how the presentation of a labial frenulum can impact future hygiene and smile. If the lip is difficult to reflect back to access the teeth so they can be brushed, the risk for plaque buildup can be increased. Lip ties do NOT cause dental decay, but the longer plaque sits on those teeth and the more carbohydrates the bacteria in the plaque have access to it can lead to demineralization (white chalky lines on teeth) and dental caries or a cavity. When plaque sits on the teeth for too long the bacteria in the plaque use these carbohydrates and produce acid. This acid will breakdown and weaken the organic structure of the enamel of the teeth and over a period of time, lead to a white, chalky line under the plaque and then decay. Proper hygiene and diet are extremely important at a young age to help minimize or avoid these problems. Starting to brush once the first tooth erupts is a good practice and seeing a pediatric dentist at or around the 1st birthday is another great way to help monitor and avoid preventable dental issues.

The picture on the left shows an upper lip that is held tight to the upper jaw when smiling the inside of the upper lip is seen and the smile shows very little gingiva. The same patient on the right side shows a thick frenulum and dental decay on the front teeth.

The same patient immediate post-frenulectomy showing a level lip position and uniform display of the gingiva. The right side shows the revision site immediate post-frenulectomy with a laser. Notice no blanching between the front teeth and fillings placed on front teeth.
Tongue Tie
Infant
What is a tongue tie?
The tongue is an extremely important, complex and still not fully understood muscle that is the first part of the gastrointestional system. It plays a major part in feeding, oral hygiene, speech and craniofacial growth and development. The tongue is made up of 8 muscles that each function in a unique manner and collectively act together as one unit. Under the tongue a piece of tissue exists in virtually all humans and is referred to as a frenulum. This piece of tissue is a remnant from the embryologic development of the tongue and normal for all individuals to have some degree or frenulum present.
Tongue frenulums can be broken down into upwards of 5 degrees or catergories, but the most important aspect is functional impairment or impact on the tongue mobility and overall function. Terms like tongue tie or tethered oral tissue (TOT) are commonly used to describe these tight or restrictive pieces of tissue. The term slight or small tongue tie is a misnomer and does not depict how well or poorly the tongue is able to function. For the purposes of simplicity these can be broken down to functional and dysfunctional tongue frenulums.
Functional Frenulums:
A functional lingual frenulum will allow for proper movement and range of motion of the tongue. It will not restrict or negatively impact surrounding structures and may or may not be visually evident. If a tongue frenulum is seen, that does not mean it is necessarily a “tie” or restricting of the tongue motion or range. On the other hand, a tongue that is able to extend out, does not necessarily mean it is functional.
Dysfunctional Frenulums or “Ties”:
Many times the symptoms being experienced by the parent and/or the child and the actual feel of the frenulum are key in helping determine if the tongue frenulum is truly tied and impacting function. More anterior ties, or that attach closer to the tip of the tongue are easy to visually diagnose, but more posterior or submucosal frenulums are not always visually evident alone.
Some individuals will have a visually evident tongue tie or restriction, but may not presently experience any symptoms or problems. These cases are still important to assess and address due to longterm issues that may impact the child, which are discussed later. A complete assessment by a well-trained lactation consultant or medical professional should be conducted to ensure compensatory mechanisms are not masking underlying problems and putting the dyad at risk for future problems.

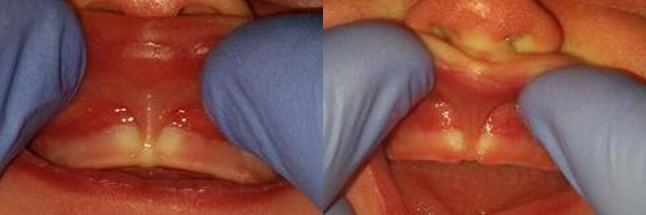
These pictures show a variety of lingual frenulums or tongue ties in infants. Notice the varied thickness, degree of webbing, connection points with the tongue and into lower jaw and restriction to tongue elevation.
Won’t the tie just stretch with time?
The frenulum is made up of fibrous tissue (Type 1 Collagen) that is equivalent to a rope. This tissue will stretch only about 3% and it is NOT a rubber band or elastic. The tongue will grow, gain more strength and mass as it is used after birth, but a restricted tongue will not spontaneously resolve in the important time period for nursing. Each frenulum will have varied lengths to it and a longer frenulum can allow a tongue to partially function, but a short and thicker frenulum, especially the submucosal variety, can have a detrimental effect on tongue mobility and function.
Nursing Challenges
Often many questions arise about what exactly is a tongue tie or lip tie is and why it occurs, how it impacts feeding in the infant and growth and development of a person over the course of their life and how can it be resolved. A major goal of this website is to help educate and allow individuals to more fully understand the implications of proper development from a very early age (as a newborn) and how proper development, growth guidance and usage of the tongue and other orofacial muscles can have a lifelong positive impact on a person. On the contrary, the non-ideal positioning and usage of the tongue and other orofacial muscles can negatively impact growth and development of the head and neck and impact the entire body.
The maxillary frenulum or lip tie rarely is a cause for nursing difficulties ALONE. The lip tie is very easy to see and diagnose, but that does not mean it is the causative factor for the nursing discomfort or problems. The tongue must groove, extend out and draw the nipple into the mouth. Once in the mouth the tongue must elevate to form the bottom half of a tube and the roof of the mouth or palate from the top of the tube. When this tube is formed a closed system is in place and the tongue should make a wave motion to propel milk out of the elongated nipple. If the infant is unable to elevate the tongue, they will close the mouth down so the tongue comes in closer proximity to the roof of the mouth. With the closing of the mouth, the initial wide gape or opening will close and the baby will slide down the areola and towards the end of the nipple. This is ineffective in milk transfer, painful for the mother and will cause the mouth to purse down to maintain an external seal. This external seal is secondary to the internal or primary seal made by the tongue. As the depth of the latch deteriorates and becomes shallower the infant will tighten the facial muscles to hold a seal and these muscle will contract. This lip contraction on the areola and nipple can lead to very sore and irritated nipples and sucking blisters and callous on the babies lips. These are not necessarily caused by a lip tie, but they are a result of a poor latch from compromised tongue function. The lip should have the ability to flange or roll back close to the nares or nostril openings with minimal resistance. The lip DOES NOT need to flange the entire way back to the tip of the nose, because the infant must be able to breathe during breastfeeding.
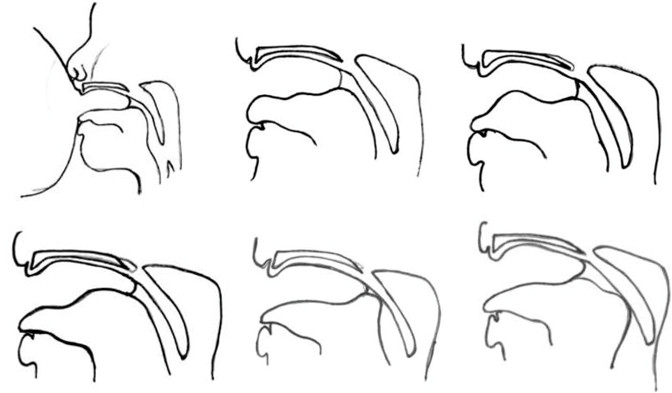
The above images show the normal progression of an infant drawing the nipple into the mouth and elongating the nipple. It also shows the wave motion that the tongue needs to produce to actively express milk from the mother. The tongue needs to elevate toward the roof of the mouth while the infant maintains a wide open gape or mouth opening. If the tongue is unable to elevate AND the mouth stay open wide, the infant will close the mouth to bring the tongue closer to the roof of the mouth. This will lead to a shallow latch, nipple compression, pain and increasing frustrations during nursing.
Stretching of the tongue revision site:
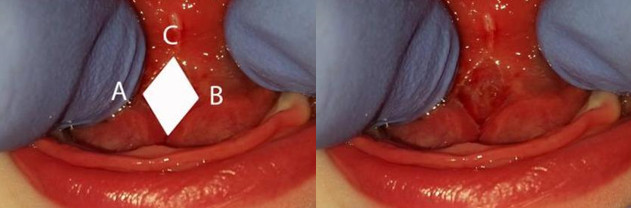
Refer to the picture of the tongue below to help outline how to do the stretches.
Gently work your finger into the mouth and under the tongue. Push into the center of the diamond until you feel some resistance or give to the tissue. Hold that depth with the finger and that move the finger from the left (Letter A) to the right (Letter B) and back in a pendulum motion. Complete 4 full pendulum swings under the tongue and over the wound site, while contacting the area under the tongue. So to review: under the tongue, A to B then B to A (repeat 3 more times). Do not remove the finger from under the tongue, but instead push the finger back and up towards letter C and hold the tongue in place for 5 seconds. This will complete the tongue stretching.
Child
What is a tongue tie?
The tongue is an extremely important, complex, and still not fully understood muscle that is the first part of the gastrointestinal system. It plays a major part in feeding, oral hygiene, speech, and craniofacial growth and development. The tongue is made up of 8 muscles that each function in a unique manner, and collectively act together as one unit. Under the tongue, a piece of tissue exists in virtually all humans, and is referred to as a frenulum. This piece of tissue is a remnant from the embryologic development of the tongue, and is normal for all individuals to have some type of frenulum present.
Tongue frenulums can be broken down into two categories: Functional, and Dysfunctional.
Functional Frenulums:
A functional lingual frenulum will allow for proper movement and range of motion of the tongue. It will not restrict or negatively impact surrounding structures and may or may not be visually evident. If a tongue frenulum is seen, that does not mean it is necessarily a “tie” or restricting the tongue’s motion or range. On the other hand, a tongue that is able to extend out, does not necessarily mean it is functional.
Dysfunctional Frenulums or “Ties”:
Many times, the symptoms being experienced by the patient, and the actual feel of the frenulum are key in helping determine if the tongue frenulum is truly tied, and impacting function. More anterior ties, or that attach closer to the tip of the tongue are easy to visually diagnose, but more posterior or submucosal frenulums are not always visually evident.
Some individuals will have a visually evident tongue tie or restriction but may not presently experience any symptoms or problems. These cases are still important to assess and address due to long-term issues that may impact the patient, which are discussed later. A complete assessment by a well-trained lactation consultant or medical professional should be conducted to ensure compensatory mechanisms are not masking underlying problems and putting the patient at risk for future problems.
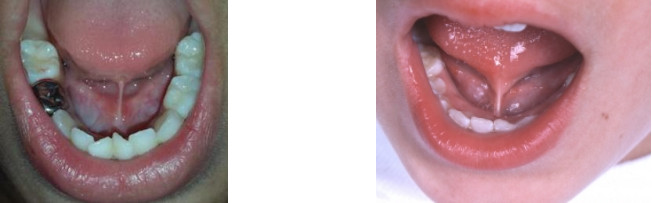
These pictures show a variety of lingual frenulums or tongue ties in children. Notice the varied thickness, degree of webbing, connection points with the tongue and into lower jaw and restriction to tongue elevation.
Won’t the tie just stretch with time?
The frenulum is made up of fibrous tissue (Type 1 Collagen) that is equivalent to a rope. This tissue will stretch only about 3% and it is NOT a rubber band or elastic. The tongue will grow, gain more strength and mass as it is used after birth, but a restricted tongue will not spontaneously resolve in the important time period for nursing. Each frenulum will have varied lengths to it, and a longer frenulum can allow a tongue to partially function, but a short and thicker frenulum, especially the submucosal variety, can have a detrimental effect on tongue mobility and function which can affect speech, growth and development, and breathing.
How does the procedure work and how long will it take?
After a thorough review of the patient’s health history, the patient will be examined. After a full evaluation and discussing treatment options, a signed consent is obtained from the parent and the procedure can proceed. The patient is taken into a treatment room with the doctor, and an assistant. The parents will wait in the exam room, and review post-operative guidelines and instructions that they are given at the appointment. The patient, doctor, and assistant will be given protective eyewear. Once all eyewear is in place, the laser is turned on. The patient’s tongue is gently elevated with a small surgical tool called a groove tongue director. It allows for the tongue to be safely elevated, and isolates the frenulum under the tongue. The type of laser we use is a CO2 laser and is able to precisely and quickly release the excessive or restrictive tissue under the tongue. The entire procedure to release the tongue is completed very quickly. Post procedural bleeding is typically very rare, but may occur, and easily managed with light pressure.